Fergus has provided a fantastic and extremely representative success story showing yet another person using lower carbs to lower their insulin as a means towards achieving normal blood sugars in their diabetes management.
Summary: Male Type 1 diabetic of 27 years
Without wishing to sound too Alcoholics Anonymous, my name is Fergus Craig, I’m a Type 1 diabetic and have been for 27 years.
Since we all suffer from a pretty similar condition, you don’t need me to remind you how it feels when you find that Mother Nature’s ripped you off, but I think I’ve learned enough to hopefully be able to offer some useful insights into my condition. The sorts of things that would have made an enormous difference to me had I figured them out much earlier than I did. In fact, over the past 7 years, I’ve been experimenting on myself to broaden my understanding. What I’ve learned has not only transformed how I deal with my condition, but rescued my health and physical fitness and probably saved my life.
I was diagnosed with acute onset Type 1 Diabetes in April 1981, as I was preparing for my end of year exams in law at University. I had all the typical symptoms of insatiable thirst, exhaustion, and extreme weight loss. As a student, more beer was the obvious solution to the first symptom. Easy. The exhaustion I put down to the work, and the weight loss I was secretly very pleased about! My doctor, however, took one look at me, sent me straight to hospital and within a week my life had changed. My exams were screwed. I started on my new life of insulin injections, urinalysis testing and a Degree in Architecture instead. Fergus Craig
If the diagnosis was quick, the coming to terms part took a great deal longer. Shamefully, I have to admit that I didn’t test my blood sugars at all for many years. Not once. I simply got by, certainly more by luck than judgement, but clearly I must have simply run my blood sugars high enough to avoid disaster, but also too high to avoid it forever. Anyone who remembers urinalysis testing will know what an effective disincentive it was to measuring the success of your treatment. It seemed to me at the time that paying attention to how you felt physically was often more informative than a test which could only really tell you when you’d screwed up, and even then only well after the event. So I simply followed my instincts, and it seemed to work reasonably well.
Over the years, however I began to notice the weight building up. The new clothes would be in slightly larger sizes than the year before despite my efforts to stay physically active but surely my diet wasn’t to blame? In time I had a beautiful wife, 4 young children and a flourishing career but still no time for my diabetes. Then, one day driving home from work my blood sugar dropped so low that I lost consciousness at the wheel of my car. I came to in the back of an ambulance with my car wrapped around a lamppost and a traffic policeman asking me whether I had intended to commit suicide. I still have a chill down my spine when I think of what might have happened. I had no recollection of even getting in the damn car, let alone the 7 miles I had travelled to get to my lamppost. That was my wake-up call.
I woke up the very next day with a to-do list that suddenly included finally facing up to the complexities of a life threatening illness, attempting to normalise my blood sugars and losing quite a few pounds in weight at the same time. Simple.
At first, I’d have been happy simply to have settled for the weight loss. I’d had enough of getting breathless climbing stairs and wobbling in an unattractive way as I came back down again. It’s not a good look. But neither could I imagine myself as the sort of person who could go hungry for very long, so the idea of ‘going on a diet’ was a bit of a non-starter. How did people do that?
Of my 27 years of diabetes, 16 of them were as a committed vegetarian. The principles of animal welfare appealed to me as a leftie student and of course it also sat comfortably with what was, and still is broadly perceived to be a healthy diet. In other words, these were 16 years in which wheat, rice and potato were the daddies. Breakfast would invariably be cereal or toast, lunch a sandwich, pizza or something under the ‘convenience’ label. Dinner of course almost invariably had to involve pasta. Oh, come on, I was a student for Christ’s sake!
None of this is a million miles away from what would be considered normal for many people in the West today. In fact, it could almost be described as low fat so would probably meet with the approval of many of the agencies that advise us on healthy living. As a student, I still had no time to test my blood sugars, so I was blissfully unaware of the affect my diet was having on my blood glucose.
However, in September 2000, I came across a newspaper article that suggested, for the first time in my experience, that the carbohydrates I’d been eating were a part of the problem – not the solution. This was just before the rebirth of the Atkins diet but the basic principles were broadly similar. They need no explanation here.
Armed with this information, I arrived home from work one evening with a shopping bag full of eggs, cream, cheese and vegetables and told my wife we were going on a diet. She thought I was joking of course, but I was deadly serious. This was a radical departure from the way I had lived previously and so at this point I was sure to weigh myself and resolved to weigh myself again every day for a year to see what happened. I would also test my blood sugar 4 to 5 times a day so I could see how my insulin needs were affected.
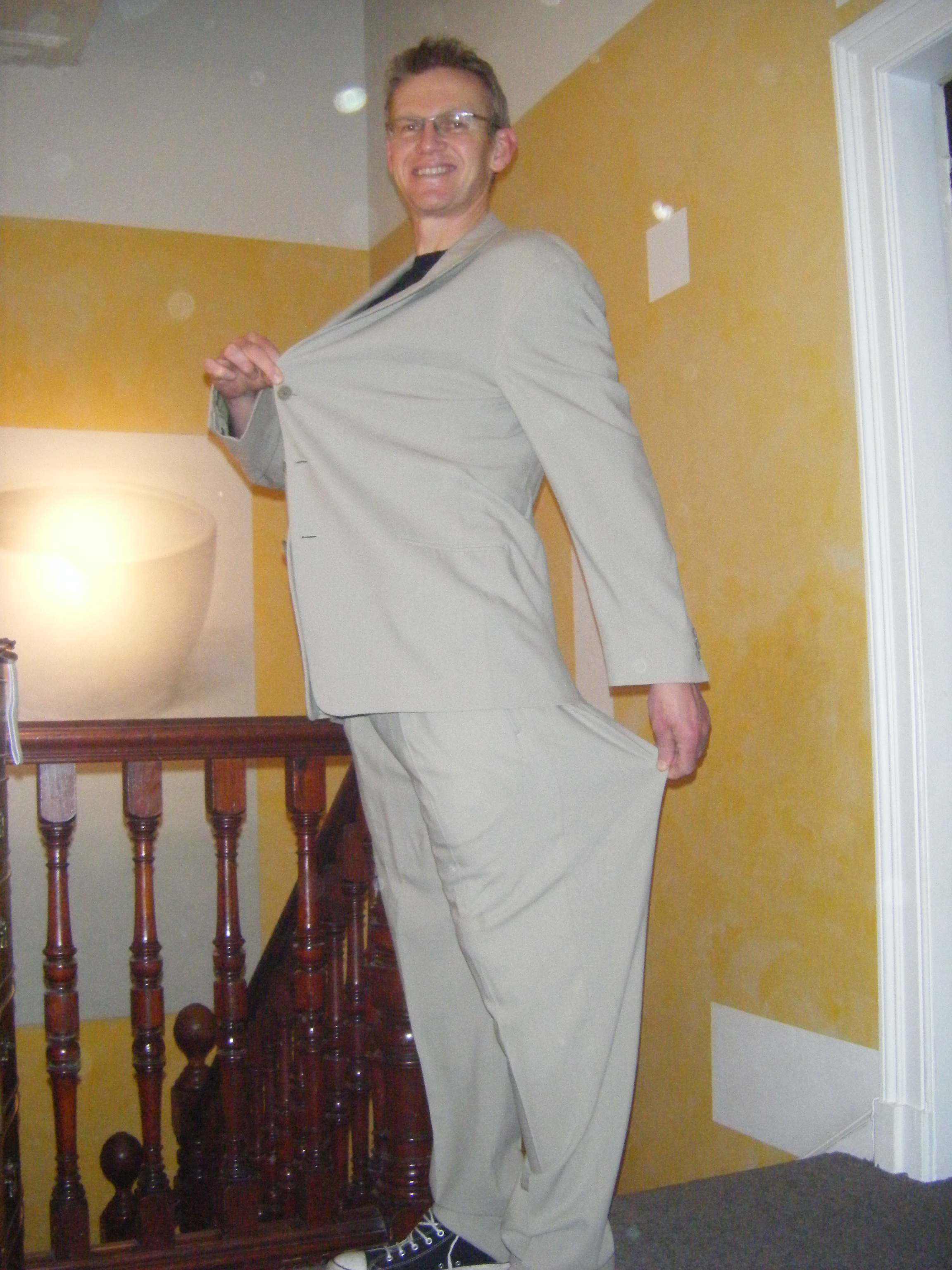
Confession time. At that time I weighed 232 pounds. For someone of my height, 6 foot 4 inches, that’s 7 pounds short of the definition of obesity. I was also injecting almost 80 units of insulin daily, which I knew had to stop.
What I observed was that the more I replaced the pasta, bread, rice and cereal with protein, vegetables and fat, the less insulin I needed. After the initial shock of deprivation of the starchy comfort food I also started to notice that I also felt hungry much less often. I made a chart. It mapped my falling weight and my falling insulin doses. The direct correlation was inescapable.
At this point something had to give if I was to replace any more of the carbohydrates with protein. It was time to ditch the vegetarian lifestyle and try and explain that one to the wife also! The look of betrayal on her face, which accompanied my first piece of salmon in 16 years, lives with me still!
So I started to eat fish again, then poultry and now the weight was really starting to shift. The bread and potatoes were slowly replaced with more green vegetables and the only real surprise was how easy the transformation was, and how much better I was starting to feel. One year after beginning the experiment, I weighed 175 pounds. My BMI had fallen from almost 29 to 22, my blood sugars were those of a healthy nondiabetic, as were my blood lipids. My friends and family were simply amazed at the transformation. I now had the energy to start cycling and running again, things I had been unable to do for years.
My daily doses of insulin, Lantus basal and Humalog bolus, had been reduced from 80 units to 21 units. I was now using 26% of the insulin I had once needed, but felt less hunger and greater energy. Even now, it seems like a deal too good to be true.
One’s glycated haemoglobin level is the best measure of longer-term blood sugar control of course. If you looked at my HbA1C chart you’d notice that, according to Dr Richard Bernstein’s research, nondiabetics who are not obese almost invariably have glycated haemoglobin level between 4.2 and 4.6%. Yet UK National Health Service guidelines have set a level of 7% as suitable for diabetics, over 50% higher than the highest nondiabetic level. These are levels far in excess of those at any time in our evolutionary history and are in fact symptomatic of the root cause of the great majority, perhaps all, of the complications associated with diabetes. I was thrilled to discover that when I replaced the starch in my diet with fat and protein, my HbA1c levels rapidly returned to a normal nondiabetic level, in the 4% range.
The reason a high HbA1C is so dangerous, I discovered, lies in the biochemistry of glucose and its interaction with proteins and lipids. The nondiabetic body reacts quickly when glucose levels are elevated in the blood and produces insulin to lower them. An appropriate analogy might be the way in which a healthy immune system produces white blood cells to combat a viral attack or infection. Excess glucose in the blood reacts chemically with proteins and destroys their ability to function. These reactions are known as glycation reactions. If these glycation reactions continue over time then they start to cause damage to all of the parts of the body normally associated with poorly controlled diabetes.
Cholesterol is often the first word I hear when I talk to people about a low carbohydrate, high fat diet. Surely high fat equals high cholesterol, which means an increased risk of cardiac problems somewhere down the line, right? Wrong. It had become clear to me that a low cholesterol diet was as logical as the low fat diet I’d followed for years. To illustrate I can offer my most recent blood test results which, after over 7 years of eating a lot more fat and a lot less carbohydrate show a higher than normal HDL (good) cholesterol and much lower than normal LDL (bad) cholesterol level. My cholesterol ratio fell from 2.6 to 1.7. My triglyceride levels are now 0.6, well below what is considered the bottom of the normal range.
Some have warned me that eating more protein in my diet risks some sort of permanent kidney damage. I see no credible evidence for this at all. In fact, a graph on the renal unit at the Edinburgh Royal Infirmary website suggests that kidney function of Type 1 diabetics is typically reduced to 33% after 25 years. That’s the about time I’ve had diabetes but my kidney function shows no sign of damage whatsoever.
It’s now clear to me that we in the developed world generally subsist on a diet that would be almost totally unrecognisable to all but our most recent ancestors. For all but the most recent 1% of our history we have thrived on a diet high in protein and fat. Carbohydrate would have formed the smallest part of our diet and at best would have comprised seasonal fruits, nuts and vegetables in very limited quantities. Carbohydrate has never been a staple food until only very recently.
There are now very few tribes of human hunter-gatherers who continue to live in ways similar to those both they and our own ancestors would have for hundreds of thousands of years. The Kung San (more familiar to us as the Bushmen of the Kalahari) has a lifestyle, and therefore a diet, reasonably close to how ours may once have been. The Kung San became something of a cause celebre in the 1960’s and 1970’s when they were one of the most extensively studied of hunter-gatherer tribes.
Although big game animals are now far less available to them than they would once have been, the Bushmen’s diet still consists predominantly of meat, milk and the fantastically exotic sounding mongongo nut. Their diet is supplemented by whatever roots, berries and vegetables are available in the immediate environment at certain times of the year. The studies (Lee) measured their food group intake as follows:
Carbohydrate- 14%
Protein- 16%
Fat- 70%
So the key thing to note is that this is an incredibly high fat diet, and relatively low in carbohydrate. Guess what happens? They are a slim and long-lived people, with no recognised incidence of cardiac illness, diabetes or many of the other diseases of the industrialised world. Now, if dietary fat was really the great evil that it is continually portrayed, wouldn’t these people show some of the symptoms of degenerative disease supposedly caused by a high fat diet? Well, they don’t, and neither do I. Nor do the Inuit, the Masai, Samburu nomads, Great Plains Indians or Australian Aborigines. They can’t all be statistical anomalies, can they?
OK, it almost feels counter-intuitive to argue for fat and protein in our diets and to say that carbohydrate is harmful and addictive. Dietary fat has had a relentlessly bad press for more than the last 30 years. At the same time that the low-fat dogma is being relentlessly and constantly reinforced, the virtues of whole grains and complex carbohydrates are held to be central to a healthy diet.
But I’d argue that even these carbs, the nice cops to refined carbohydrates nasty cops, are comparative newcomers to the human diet. Before the agricultural revolution some 8 – 10,000 years ago these foods were not part of our diet at all. Our bodies simply haven’t had sufficient time to learn how to deal with them properly. But particularly as we now consume them in unprecedented quantities so we find crises of diabetes and obesity as never before.
The role of the hormone insulin is key to resolving these issues. In that sense, my ability precisely to measure and control my insulin usage, and to correlate that with my weight and my blood lipid profile, has proven to me beyond doubt that neither fat, saturated or unsaturated, nor protein causes us harm. It’s the carbohydrate, and the disproportionate quantity of insulin required to deal with it, that harms us. By us, I mean all of us and not simply the diabetic minority.
I have proven to myself that in dramatically reducing my consumption of carbohydrates, I have made a correspondingly dramatic reduction in my insulin requirements. This has equated to a return to my optimum body weight and to a blood lipid profile that very few nondiabetics could aspire to.
Unless I was an insulin dependant diabetic, I doubt I would have been able to make this clear association between insulin usage and physical health. In that sense, it’s a great privilege to be diabetic.
It’s fairly clear from my measurements that reducing my insulin usage, normalising my blood sugars and keeping them controlled has resulted in significant weight loss. Not only that, but it has achieved the even harder task of maintaining that weight loss.
My self-experimentation has convinced me that we are privileged to live in an era when we not only have the treatments available to help us lead normal lives, but also that the tools at our disposal allow us an understanding of our dietary processes which is denied to the vast majority of ‘normal’ people.
I’ve come a long way since September 2000. The principles I have learned have rescued my health and given me the tools I need to lead a long, healthy active life, unencumbered by my diabetes. I have no diabetic complications at all, which may be unusual for someone who has had the condition for such a long time. My only regret is that the medical establishment is so entrenched in its own dietary dogma that it cannot or will not recognise the simple truths that could make such a difference to the lives and the health of so many.
My sincere wish is that the medical experts who offer advice to diabetics and non-diabetics alike will recognise the great benefits that a low carbohydrate lifestyle can bring and many more people may enjoy those benefits too.
Fergus Craig
December 2007 Copyright for this article and all its contents remains with Fergus Craig.